Why the recurrence?
Inflammation is the key. The source of inflammation comes from dry eyes and meibomian gland dysfunction (MGD). Treating it at the same time with dry eyes and MGD will stop its recurrence. Treating all three (3) condition is the approach TheraLife takes, and we have been very successful.
To learn more, click here.
What is it?
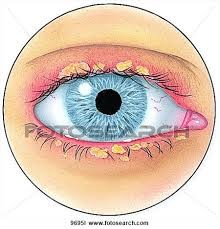
Blepharitis is a common condition that causes inflammation of the eyelids. The situation can be challenging to manage because it tends to recur.
What are other associated eye conditions ?
Complications from blepharitis include:
Stye: A red bump on the eyelid. Bacterial infection of the oil glands of the eyelid causes the stye. The reason for a stye is due to clogged oil glands, MGD.
Chalazion: This condition is often confused with the stye.
A stye is infectious, and chalazion is not. It is a usually painless firm lump caused by inflammation of the oil glands of the eyelid. A chalazion can be painful and red and will often go away by itself.
Tear Film Abnormality: Abnormal or decreased oil secretions (MGD) that are part of the tear film can result in excess tearing ( Watery Dry Eyes ) or dry eye.
Because tears are necessary to keep the cornea healthy, tear film problems can make people more at risk for corneal damage or infections (Conjunctivitis).
Causes
There are two forms:
Anterior blepharitis affects the outside front of the eyelid, where the eyelashes are attached. The two most common causes of anterior blepharitis are bacteria (Staphylococcus), scalp dandruff, and mites (Demodex)
Posterior blepharitis affects the inner eyelid (the moist part that makes contact with the eye). The oil (meibomian) glands in this part of the eyelid are the problem.
Two skin disorders can cause this form of blepharitis: acne rosacea, which leads to red and inflamed skin, and scalp dandruff (seborrheic dermatitis).
Symptoms
Symptoms of blepharitis include a foreign body or burning sensation; excessive tearing; itching, sensitivity to light (photophobia); red and swollen eyelids; redness of the eye; blurred vision; frothy tears; dry eye; or crusting of the eyelashes on awakening (eyeballs stuck to the eyelids).
These symptoms are similar to chronic dry eyes except in blepharitis; the eyelid has sticky crusty build up.
Treatments
Treatment for both forms of blepharitis involves keeping the lids clean and free of crusts. Apply warm compresses to the eyelid to loosen the crusts, followed by a light scrubbing of the eyelid with a cotton swab and eyelid cleanser.
We highly recommend Avenova. Because blepharitis rarely goes away completely, most people must maintain an eyelid hygiene routine for life. If the blepharitis is severe, an eye doctor may also prescribe antibiotics or steroid eyedrops.
When scalp dandruff is present, use a dandruff shampoo for the hair. In addition to the warm compresses, patients with posterior blepharitis will need to massage their eyelids to clean the glands’ oil. Patients who also have acne rosacea should have that condition treated at the same time.
How Theralife can help
Check out the TheraLife all-in-one treatment starter kit. Total relief for dry eye related problems in one concise protocol.
100% money back guaranteed.
Here is a video on how to massage eyelids after a hot compress. Click here
It is time to maintain your eye health, relieve dry eyes, and keep blepharitis at bay.
Courtesy: National Eye Institute, National Institutes of Health (NEI/NIH)
The National Eye Institute (NEI) is part of the National Institutes of Health (NIH) and is the Federal government’s lead agency for vision research that leads to sight-saving treatments and plays a key role in reducing visual impairment and blindness.
Personal story of Blepharitis recovery with TheraLife
Blepharitis MGD Recovery
I have had blepharitis that would come concurrent with pink eye for quite a few years, but it has always gone away pretty quickly on its own. This last time, however, blepharitis and dry eye did not leave, and it became quite disruptive to my life.
My eye doctor gave me eye drops, which only made my eyes feel more dry. I felt as though I had no hope for my eyes and they were just going to keep getting worse and worse.
I finally decided to try Theralife, despite being fairly skeptical, and I’m So glad I did. I’ve now been taking it for just over two weeks, and I already feel so much better. This morning I woke up and my eyes were almost white, instead of bright red.
My blurry Vision is pretty much cleared up, the stickiness gone from eye, and the stinging has almost left. I’m looking forward to them getting better and better. Thanks so much!”
Cindy, USA
- Results ,may vary
References
- 1.
- Huggins AB, Carrasco JR, Eagle RC. MEN 2B masquerading as chronic blepharitis and euryblepharon. Orbit. 2019 Dec;38(6):514-518.
- 2.
- Rodriguez-Garcia A, Loya-Garcia D, Hernandez-Quintela E, Navas A. Risk factors for ocular surface damage in Mexican patients with dry eye disease: a population-based study. Clin Ophthalmol. 2019;13:53-62. [
- 3.
- Choi FD, Juhasz MLW, Atanaskova Mesinkovska N. Topical ketoconazole: a systematic review of current dermatological applications and future developments. J Dermatolog Treat. 2019 Dec;30(8):760-771.
- 4.
- Ozkan J, Willcox MD. The Ocular Microbiome: Molecular Characterisation of a Unique and Low Microbial Environment. Curr Eye Res. 2019 Jul;44(7):685-694.
- 5.
- Khoo P, Ooi KG, Watson S. Effectiveness of pharmaceutical interventions for meibomian gland dysfunction: An evidence-based review of clinical trials. Clin Exp Ophthalmol. 2019 Jul;47(5):658-668.
- 6.
- Soh Qin R, Tong Hak Tien L. Healthcare delivery in meibomian gland dysfunction and blepharitis. Ocul Surf. 2019 Apr;17(2):176-178.
- 7.
- Fromstein SR, Harthan JS, Patel J, Opitz DL. Demodex blepharitis: clinical perspectives. Clin Optom (Auckl). 2018;10:57-63.
- 8.
- Pflugfelder SC, Karpecki PM, Perez VL. Treatment of blepharitis: recent clinical trials. Ocul Surf. 2014 Oct;12(4):273-84.
- 9.
- Kanda Y, Kayama T, Okamoto S, Hashimoto M, Ishida C, Yanai T, Fukumoto M, Kunihiro E. Post-marketing surveillance of levofloxacin 0.5% ophthalmic solution for external ocular infections. Drugs R D. 2012 Dec 01;12(4):177-85.
- 10.
- Veldman P, Colby K. Current evidence for topical azithromycin 1% ophthalmic solution in the treatment of blepharitis and blepharitis-associated ocular dryness. Int Ophthalmol Clin. 2011 Fall;51(4):43-52. [PubMed]
- 11.
- Hosseini K, Bourque LB, Hays RD. Development and evaluation of a measure of patient-reported symptoms of Blepharitis. Health Qual Life Outcomes. 2018 Jan 11;16(1):11.
*GRADE: Grading of Recommendations Assessment, Development and Evaluation (www.gradeworkinggroup.org)
Sources of evidence
Amescua G, Akpek EK, Farid M, Garcia-Ferrer FJ, Lin A, Rhee MK, Varu DM, Musch DC, Dunn SP, Mah FS; American Academy of Ophthalmology Preferred Practice Pattern Cornea and External Disease Panel. Blepharitis Preferred Practice Pattern®. Ophthalmology. 2019;126(1):P56-P93
Bilkhu PS, Naroo SA, Wolffsohn JS. Randomised masked clinical trial of the MGDRx EyeBag for the treatment of meibomian gland dysfunction-related evaporative dry eye. Br J Ophthalmol. 2014;98(12):1707-11
Cote S, Zhang AC, Ahmadzai V, Maleken A, Li C, Oppedisano J, Nair K,
Busija L, Downie LE. Intense pulsed light (IPL) therapy for the treatment of
meibomian gland dysfunction. Cochrane Database of Systematic Reviews
2020, Issue 3. Art. No.: CD013559Geerling G, Tauber J, Baudouin C, Goto E, Matsumoto Y, O’Brien T, Rolando M, Tsubota K, Nichols KK. The International Workshop on Meibomian Gland Dysfunction: Report of the Subcommittee on Management and Treatment of Meibomian Gland Dysfunction. Inv Ophthalmol Vis Sci. 2011;52(4):2050-2064
Jones L, Downie LE, Korb D, Benitez-Del-Castillo JM, Dana R, Deng SX, Dong PN, Geerling G, Hida RY, Liu Y, Seo KY, Tauber J, Wakamatsu TH, Xu J, Wolffsohn JS, Craig JP. TFOS DEWS II Management and Therapy Report. Ocul Surf. 2017;15(3):575-628
Kashkouli MB, Fazel AJ, Kiavash V, Nojomi M, Ghiasian L. Oral
azithromycin versus doxycycline in meibomian gland dysfunction: a
randomised double-masked open-label clinical trial. Br J Ophthalmol.
2015;99(2):199-204Lindsley K, Matsumura S, Hatef E, Akpek EK. Interventions for chronic blepharitis. Cochrane Database of Systematic Reviews 2012, 5: CD005556
Navel V, Mulliez A, Benoist d’Azy C, Baker JS, Malecaze J, Chiambaretta
F, Dutheil F. Efficacy of treatments for Demodex blepharitis: A systematic
review and meta-analysis. Ocul Surf. 2019; 17(4):655-669Pflugfelder SC, Karpecki PM, Perez VL. Treatment of blepharitis: recent clinical trials. Ocul Surf. 2014;12(4):273-84
Sabeti S, Kheirkhah A, Yin J, Dana R. Management of meibomian gland
dysfunction: a review. Surv Ophthalmol. 2019 Sep 5. pii: S0039-
6257(19)30253-X. doi: 10.1016/j.survophthal.2019.08.007. [Epub ahead of
print]Sung J, Wang MTM, Lee SH, Cheung IMY, Ismail S, Sherwin T, Craig JP. Randomized double-masked trial of eyelid cleansing treatments for blepharitis. Ocul Surf. 2018;16(1):77-83
Zhao YE, Wu LP, Hu L, Xu JR. Association of Blepharitis with Demodex: A Meta-analysis. Ophthalmic E