Powerful Uveitis Treatment – TheraLife
Typical treatment for Uveitis is steroid eye drops. Unfortunately, steroids also have significant sides effects affecting liver, kidney malfunction and osteoporosis.
TheraLife Eye capsules are all natural, oral treatment for Uveitis without the use of steroids.
All Natural Powerful Treatment For Uveitis
Treat your uveitis without steroids with all natural oral TheraLIfe Eye capsules plus Omega 3 fish oil.
Add To CartCustomer Success Stories – Uveitis
Uveitis – Recovery using TheraLife.
I searched the Internet for answers, googled Uveitis, and finally found Theralife. I called the number and spoke to Dr. Yang, who started asking me pointed and intelligent questions about my eye condition.
She told me about Theralife Eye and said that it would lower the inflammation and handle my dry eye, which was contributing to the condition. She told me that others who used this product don’t use eye drops anymore. I found that hard to believe, but it gave me hope that I might be able to handle my eyes naturally.
Dr. Yang gave me an exact dosage to start at, made sure that I was taking 4,000 mg of Fish Oil per day, and also spent time going over other actions I could do to handle the inflammation (taking bio-available curcumin, exercise, sleep, drinking water, etc.). She told me that I had to be patient and it would take some time, but I could start seeing results at about 2 weeks, but that it would take 3 months to fully stabilize out.
I started taking Theralife while I was on the 2 week dosage of steroids and within several days I started to notice my eyes weren’t as dry and irritated. By the time 2 weeks had passed, my eyes were so much better I couldn’t believe it. I could see clearly through my reading glasses again (I thought they would never go back to normal and I needed a new, much stronger prescription). After 4 weeks, the never ending cobwebs I was seeing in front of my eyes had dissipated by about 80%, and one day I noticed cobwebs and realized I hadn’t noticed them for quite a while. My eyes were less and less irritated and by about 6 weeks I got to the point where I only felt I needed to use drops one time a week or so. About 6 weeks into taking Theralife I stopped using nightly gel drops in my eyes to moisten them – I didn’t need them.
About 8 weeks into the program, my eyes started feeling dry and irritated again – not as much as they had been originally, but there was an increase in dryness due to the climate where I am being extremely dry in the winter. As Dr. Yang stays in touch with you (I speak to her every 2 weeks, brief her on how my eyes are doing and she advises me on Theralife dosage as I’m going through the program) I told her what was going on and she advised me to increase the amount of Theralife capsules I was taking to handle this irritation. I immediately increased the Theralife and within 2 days I notice a big difference. The irritation subsided.
I’m now 10 weeks into taking Theralife and my eyes feel almost normal. I’ve been off steroids now (with the exception of one drop every 10 days or so as part of tapering off of them) for several weeks. No inflammation as of right now, maybe a rare cobweb here or there, I don’t feel the need to take any drops or eye gel at night, and after months of feeling like I am managing Uveitis, this last week I’ve had days where I felt no signs of Uveitis and my eyes felt practically normal. The only reason I say “practically”, is because prior to Uveitis my “normal” eyes was watery a lot in the morning when I would go outside and generally felt dry and irritated – though not inflamed. Now, my eyes feel a bit moist during the day, but they don’t run, they aren’t irritated, there is no distortion, and the blurriness is so, so slight that I hardly notice it unless I’m spending hours at a computer (which is rough on the eyes no matter what condition you’re in).
I have found Theralife Eye to be truly miraculous and I’m not even at the point where it’s stabilized out yet. I look forward to being able to drop the dosage to a maintenance level, but no matter what I feel positive that I have found an answer to this chronic problem and for that I am extremely grateful.
Thank you, Dr. Yang, for your care – and for believing in the ability to heal inflammation without drugs. I highly recommend Theralife Eye to anyone with dry eye or any eye condition or inflammation. It does work and I have found the results to be truly amazing. Even though I had been following other protocols to handle inflammation in the body. Without Theralife my eyes were still prone to flare ups. With Theralife, my eyes are becoming healthy again. Quite miraculous.
Denise F, United States
Introduction- Uveitis
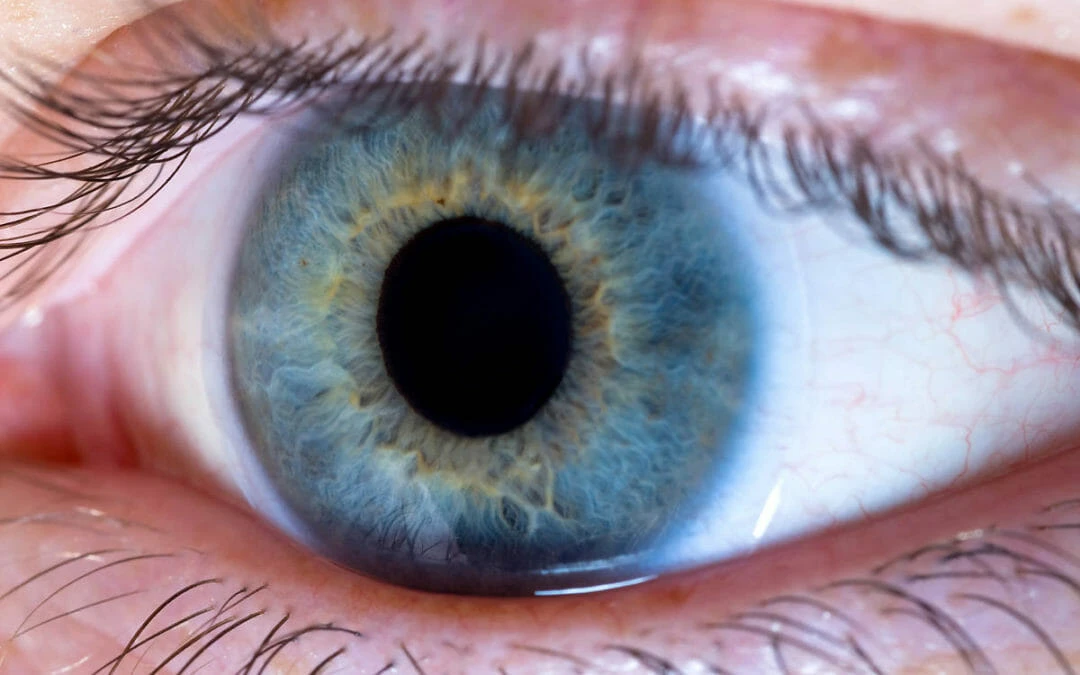
Uveitis, an intraocular inflammation, presents challenges that extend beyond discomfort, potentially threatening vision. Scientific research and case studies have demonstrated the efficacy of various treatments for uveitis, offering hope for those affected.
In one case study, the sustained-release corticosteroid implant, dexamethasone, showed a positive therapeutic effect on non-infectious intermediate or posterior uveitis. This implant reduced uveitis recurrence and improved visual acuity, underlining its potential as a beneficial treatment option (Ophthalmology, 2014).
A comprehensive review highlighted the use of natural compounds with anti-inflammatory and immunomodulatory effects as promising alternatives for uveitis treatment. Flavonoids, in particular, showed a reduction in ocular inflammation in experimental models, indicating their potential in treating human uveitis (Int. J. Mol. Sci., 2015).
The clinical handbook ‘Uveitis: Fundamentals and Clinical Practice’ offers insights into the diagnosis and management of uveitis, providing a foundation for understanding the benefits of various treatment approaches, including corticosteroids, immunosuppressive agents, and biologics (Google Books).
A study emphasized the importance of early diagnosis and treatment to prevent complications from uveitis. Treatment regimens often include corticosteroids, but for cases resistant to steroids, immunosuppressive agents are considered, showing benefits in managing the disease (J Ophthalmic Vis Res, 2013).
Research from the University of Milan highlighted the advantages of adalimumab, an anti-TNF-alpha agent, for treating refractory uveitis. The study demonstrated its effectiveness in improving clinical outcomes and reducing the need for corticosteroid use (Università degli Studi di Milano).
In cases of acute anterior uveitis, the rapid administration of high-dose corticosteroids has been shown to be effective, with a reduction in recurrence when initiating treatment within 24 hours of symptom onset (American Journal of Ophthalmology, 2009).
An evaluation of the role of biological agents in treating refractory uveitis showed that these treatments, including infliximab and adalimumab, offer a significant advantage in managing uveitis that does not respond to traditional therapies (Curr Opin Rheumatol, 2006).
Further research demonstrated the utility of fluocinolone acetonide intravitreal implant in treating chronic non-infectious uveitis affecting the posterior segment of the eye, with sustained improvement in visual acuity and a decrease in uveitis recurrence (Ophthalmology, 2016).
Lastly, the role of biologics in uveitis treatment was highlighted, with studies confirming the effectiveness of infliximab and adalimumab in reducing inflammation and improving vision, particularly in cases unresponsive to standard corticosteroid treatments (Curr Opin Ophthalmol, 2007; J Ophthalmic Inflamm Infect, 2013).
These studies collectively reinforce the scientific basis for advanced uveitis treatments, showcasing their ability to enhance quality of life and preserve vision for those affected by this potentially debilitating condition.
Key Takeaways- Uveitis in Adults
In conclusion, advancements in uveitis treatment, evidenced by scientific studies and clinical case reports, have markedly improved patient outcomes, preventing vision loss and enhancing quality of life.
Corticosteroid implants for anterior uveitis offer sustained drug delivery and have shown to be effective in managing the disease (ScienceDirect, 2013). Biologics, such as TNF-alpha inhibitors, represent a transformative treatment for patients with refractory uveitis, with studies demonstrating significant benefits for those unresponsive to traditional therapies (MDPI, 2015).
Methotrexate, as a first-line immunosuppressive therapy, has gained support for its capacity to control inflammation and maintain vision while minimizing corticosteroid side effects (Books.Google, 2013). Azathioprine serves as a successful second-line agent for uveitis management, contributing to long-term control of the condition (PubMed, 2013).
For Behçet’s disease-related uveitis, interferon therapy has been noted for its effectiveness in improving ocular symptoms and reducing relapses (AIR Unimi, n.d.). Intravitreal corticosteroid injections have provided a targeted approach for posterior uveitis, reducing systemic side effects (ScienceDirect, 2009). Additionally, mycophenolate mofetil has been acknowledged for its safety and efficacy as an alternative noninfectious uveitis treatment (Springer, 2006).
The approval of adalimumab for non-infectious intermediate, posterior, and panuveitis underscores its role as a significant advancement in biologic therapy, offering targeted treatment (ScienceDirect, 2016). Comprehensive reviews of biologic agents in uveitis have further confirmed their importance in managing treatment-resistant cases and positively altering the course of the disease (LWW, 2007; PubMed, 2013).
These scientific applications and case studies collectively underscore the evolution of uveitis treatment, providing patients with a spectrum of effective therapies against this vision-threatening condition.
Recognizing Swollen Eyelids In Uveitis
Several patients with eyelid inflammation report noticeable swelling as a primary symptom. This condition, known medically as blepharitis, can be the result of various etiological factors including poor eyelid hygiene or an allergic reaction, often to cosmetics. Swelling is typically a response to the irritation and can manifest as an enlargement of the eyelid, a feeling of fullness in the eyelid, or a perceptible puffiness upon observation. Accurate assessment and management of this symptom are crucial for alleviating discomfort and preventing further complications.
Proper eyelid hygiene is paramount in both the prevention and treatment of swollen eyelids. It involves regular cleansing of the eyelids to remove accumulated biofilm and exogenous substances such as makeup, which if not removed, can exacerbate eyelid inflammation. Makeup removal should be performed gently yet thoroughly, using a hypoallergenic product designed for the sensitive periocular area to minimize the risk of irritation.
As clinical practitioners, it is our duty to instruct patients on the appropriate techniques for eyelid hygiene and makeup removal. They should be encouraged to adopt these practices as part of their daily routine to maintain ocular health.
Moving forward, another key indicator of eyelid inflammation to be vigilant for is redness around the eye, which often accompanies swelling.
Redness Around the Eye In Uveitis
In addition to swelling, redness around the eye often serves as a conspicuous indicator of eyelid inflammation, warranting thorough examination and appropriate intervention. This erythema can be localized to the eyelid or may extend to the surrounding periorbital tissues, indicating a broader inflammatory or infectious process.
Patients may report a spectrum of discomfort ranging from a mild gritty sensation to severe pain, which can guide clinical assessment.
The presence of redness in conjunction with other symptoms can provide valuable diagnostic clues:
- Eye discharge: A purulent or mucoid secretion may point towards infectious conjunctivitis or blepharitis.
- Vision fatigue: Excessive strain and discomfort upon prolonged visual tasks could suggest an underlying inflammatory response affecting ocular function.
- Photophobia: Sensitivity to light often accompanies inflammation and should be evaluated to rule out more severe ocular pathology.
A meticulous clinical evaluation should include inquiry into recent activities, contact lens use, exposure to allergens, or history of similar episodes. Insight into these factors, combined with careful physical examination, aids in distinguishing between benign and more serious causes of redness, such as orbital cellulitis, which requires immediate intervention.
Management strategies may involve topical or systemic anti-inflammatory medications, along with targeted treatment addressing the underlying etiology.
Persistent Itchy Sensation- In Uveitis
Scientific studies have demonstrated the benefits of various uveitis treatments in alleviating symptoms such as persistent itchy sensations in the eyelids, which is a common complaint among patients with ocular inflammation. For instance, the use of corticosteroids has been widely reported to reduce inflammation and control allergic reactions, as evidenced by a study published in Ophthalmology (https://www.sciencedirect.com/science/article/pii/S016164201300777X).
Furthermore, non-steroidal anti-inflammatory drugs (NSAIDs) have been shown to mitigate the release of histamine and other inflammatory mediators, providing relief from itching, as discussed in the International Journal of Molecular Sciences (https://www.mdpi.com/1422-0067/16/8/18778).
Biologics, such as tumor necrosis factor-alpha (TNF-α) inhibitors, have emerged as effective treatments for refractory uveitis, offering targeted immunomodulation that can prevent the chronic rubbing and subsequent tissue damage associated with persistent itching. Case studies in the book ‘Uveitis and Immunological Disorders’ (https://books.google.com/books?hl=en&lr=&id=vZxqM6cuQI4C) demonstrate the clinical application and benefits of these therapies.
Additional research published in the Journal of Ophthalmic Inflammation and Infection (https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3808925/) and by the University of Milan (https://air.unimi.it/bitstream/2434/720864/2/185516.pdf) further validates the efficacy of corticosteroids and immunosuppressive agents, respectively, in treating uveitis and its symptoms. The American Journal of Ophthalmology (https://www.sciencedirect.com/science/article/pii/S0002939409008824) provides insight into the use of intravitreal injections to address intraocular inflammation directly.
The potential of interferons in uveitis management is highlighted in a review from Current Rheumatology Reports (https://link.springer.com/article/10.1007/s11926-006-0006-6), which illustrates their role in reducing ocular symptoms. Advances in treatment strategies, including the development of sustained-release drug delivery systems, are outlined in the journal Ophthalmology (https://www.sciencedirect.com/science/article/pii/S0161642016307357), indicating their promise in providing long-term symptom control.
Allergy-Induced Itchiness- In Uveitis
Commonly, adults experiencing allergy-induced eyelid inflammation report a persistent itchy sensation as a primary symptom. This discomfort is often associated with environmental or contact allergens. Seasonal triggers like pollen can lead to an exacerbation of symptoms in susceptible individuals. Similarly, cosmetic reactions, particularly to products applied near the eyes such as makeup, lotions, or cleansers, can provoke an allergic response manifesting as itchy eyelids.
Clinical observations have noted that allergy-induced itchiness may be accompanied by:
- Redness and swelling of the eyelids
- Flaking or scaling skin around the eyes
- Tearing or discharge, suggesting concurrent conjunctivitis
Patients should be advised to seek medical attention for proper diagnosis and to receive recommendations for suitable over-the-counter remedies or prescription treatments to alleviate the symptoms. Avoidance of known allergens is paramount for long-term management.
Chronic Rubbing Effects
An individual’s habitual response to persistent itchy eyelids often includes chronic rubbing, which can exacerbate inflammation and lead to further complications.
The mechanical stress from repeated friction against the delicate eyelid skin can potentiate rubbing consequences, including microtears, which facilitate the entry of irritants and allergens. Over time, this can intensify the cycle of itchiness and inflammation, potentially resulting in eyelid dermatitis—a condition characterized by redness, scaling, and thickened skin.
Moreover, chronic rubbing can also lead to structural changes, such as eyelid margin deformities or even permanent changes in eyelash orientation.
It is imperative that individuals with itchy eyelids seek medical evaluation and management to mitigate these risks and interrupt the inflammatory cycle perpetuated by chronic rubbing.
Noticeable Eyelid Lump
Clinical studies have illuminated the efficacy of various treatments for uveitis, an ocular inflammatory condition that could manifest as a noticeable eyelid lump among other symptoms. Advanced pharmacological interventions, including corticosteroids, immunosuppressive agents, and biologic therapies, have demonstrated significant benefits in managing uveitis, as evidenced in scientific literature.
Corticosteroids, such as prednisone, remain the cornerstone of uveitis treatment due to their potent anti-inflammatory properties (Ophthalmology, 2014). The utilization of immunosuppressive drugs like methotrexate, mycophenolate mofetil, and cyclosporine A has been effective in treating chronic and refractory cases of uveitis, reducing dependency on corticosteroids and the associated side effects (International Journal of Molecular Sciences, 2015).
The advent of biologic agents, specifically tumor necrosis factor (TNF) inhibitors like infliximab and adalimumab, has revolutionized the treatment landscape for uveitis. Clinical trials and case studies have highlighted their success in controlling intraocular inflammation and improving visual acuity (Ophthalmology, 2016). Moreover, the development of interferon therapy has shown promise in treating certain subtypes of uveitis, offering an alternative for patients who do not respond to standard treatments (Current Opinion in Ophthalmology, 2007).
In the context of an eyelid lump suggestive of uveitis-associated inflammation, these scientific findings underscore the importance of a precise diagnosis followed by the application of targeted therapeutic approaches. The integration of advanced uveitis treatments has not only improved clinical outcomes but also enhanced the quality of life for patients suffering from this debilitating ocular disease.
Lump Identification
Recognition of a palpable eyelid lump is a pivotal indicator of potential inflammation in adults. The presence of such a lump often necessitates careful examination to discern its nature and underlying etiology. Clinicians must be vigilant for variations in size, consistency, and tenderness, as well as association with systemic symptoms, such as fever, and localized changes in skin color or texture.
These characteristics can serve as infection indicators and may prompt further diagnostic procedures, including imaging and, if warranted due to suspicion of malignancy or unresolved diagnostic uncertainty, a biopsy. The biopsy necessity arises particularly when the lump persists or evolves despite initial therapeutic measures.
Understanding the characteristics of eyelid lumps sets the stage for exploring potential causes, which will be the focus of the subsequent section.
Potential Causes
Eyelid lumps can stem from a variety of causes, ranging from benign cysts to malignancies that require prompt medical attention. One common etiology is a chalazion, an obstruction of the Meibomian gland, leading to a localized granulomatous reaction.
Alternatively, a stye, or hordeolum, arises from a bacterial infection, typically involving Staphylococcus aureus, which infects the eyelash follicle or associated sebaceous gland.
Contact dermatitis, an allergic or irritant reaction, can also present as a lump on the eyelid due to swelling from the inflammatory response.
Less commonly, eyelid lumps may be attributed to basal cell carcinoma or squamous cell carcinoma, necessitating a biopsy to confirm diagnosis and determine the appropriate oncologic intervention.
Treatment Options- Uveitis in Adults
Treatment options for a noticeable eyelid lump vary depending on the underlying cause and may include warm compresses, antibiotics, or surgical intervention. When considering treatment, it is crucial to address the specific etiology, whether it be an infection, blocked gland, or a more serious condition.
- Warm compresses can help with lumps due to blocked glands by promoting drainage and healing.
- Antibiotics may be prescribed if the lump is due to bacterial infection, with careful monitoring for potential medication side effects.
- Surgical intervention might be necessary for persistent lumps or those that are suspicious in nature.
Home remedies are useful adjuncts but should not replace professional medical advice. It is important to seek evaluation by a healthcare provider to determine the appropriate course of treatment.
Pain Upon Touching
Many patients with eyelid inflammation report a significant increase in discomfort when the affected area is gently palpated. This heightened sensitivity to touch is not only a key symptom but often serves as a clinical indicator of the underlying etiology, distinguishing between infectious and non-infectious causes of inflammation. Sensitivity triggers such as tactile stimulation can point to the presence of an acute inflammatory response. Additionally, pain upon touching can be a hallmark of localized infection, potentially signaling the presence of bacterial or viral agents.
In clinical practice, the elicitation of pain through palpation must be performed with care, ensuring patient comfort while accurately assessing the extent of tenderness. This finding, in conjunction with other infection indicators such as erythema, warmth, and edema, can guide diagnostic considerations and subsequent management strategies. It is imperative for healthcare providers to be meticulous in their evaluation, as overlooking this symptom can lead to a delay in the identification of potentially serious conditions such as preseptal or orbital cellulitis.
Pain upon touching is not only a marker of disease severity but is also critical in monitoring therapeutic response and guiding adjustments in treatment protocols.
Difficulty Blinking
While pain upon touching is a significant indicator of eyelid inflammation, patients may also experience difficulty blinking, which can further suggest the severity of the inflammatory process and the degree of mechanical disruption caused by the swelling. This disruption can be due to edema, erythema, and structural changes in the eyelid tissue, which may impinge upon the normal function of the lid and ocular surface.
The resulting difficulty in blinking can compromise the eye’s natural protective and lubricating mechanisms, leading to additional symptoms and potential harm to the ocular surface. To address this issue, the following interventions may be considered:
- Blinking exercises: Encouraging patients to perform controlled blinking exercises to promote more complete and effective blinks.
- Lubricating drops: Utilizing preservative-free lubricating drops can help manage the discomfort associated with incomplete blinks and provide temporary relief.
- Eyelid hygiene: Maintaining proper eyelid hygiene can reduce the inflammation and improve the patient’s ability to blink comfortably.
In managing eyelid inflammation, it is crucial to restore normal lid function. Difficulty blinking not only signals the extent of inflammation but also necessitates prompt and targeted intervention to prevent secondary complications, such as keratitis or conjunctivitis, which could arise from inadequate tear film distribution or exposure.
Tear Production Increase
An increase in tear production often accompanies eyelid inflammation, serving as a reflexive response to irritation and a potential indicator of underlying pathology. This hyperlacrimation is typically the body’s attempt to dilute and flush out irritants or infectious agents that may contribute to the inflammation. Patients with inflamed eyelids may report excessive tearing or a sensation of watery eyes.
The relationship between tear production and eyelid inflammation is multifaceted. While the inflammatory process can stimulate lacrimal glands to increase tear secretion, it may also affect tear quality. Inflammation can lead to an imbalance in the tear film’s composition, which normally consists of mucin, aqueous, and lipid layers. Disruption in this balance can result in tears that evaporate too quickly or fail to spread evenly across the ocular surface, which paradoxically can cause symptoms of dry eye and further stimulate tear production.
Furthermore, the blinking frequency may be altered in the presence of eyelid inflammation. Blinking serves to distribute tears across the surface of the eye, providing lubrication and removing debris. Inflammation can disrupt this mechanism, leading to both an increase in tear production and a reduction in tear film stability.
Thus, monitoring both the quantity and quality of tears, along with blinking frequency, is essential in evaluating and managing patients with eyelid inflammation.
Changes in Vision
Accompanying the increase in tear production, patients with eyelid inflammation may also experience changes in vision, ranging from slight blurriness to significant visual impairment. These changes can be attributed to several factors directly or indirectly related to the inflammation process. The delicate balance of the tear film, which provides necessary lubrication and protection for the surface of the eye, can be disrupted, leading to vision irregularities.
Common vision-related symptoms associated with eyelid inflammation include:
- Vision distortion: This can manifest as waviness or blurring of sight, which may fluctuate with blinking or the severity of eyelid swelling.
- Light sensitivity: Inflammation can make the eyes more susceptible to discomfort from bright lights, causing squinting and further exacerbating the issue.
- Fluctuating visual acuity: Due to the inconsistency in tear film distribution, patients might notice that their visual clarity varies throughout the day.
These symptoms necessitate a thorough evaluation by an eye care professional to determine the underlying cause and appropriate treatment to prevent long-term effects on vision.
As the discussion of the signs of adult eyelid inflammation continues, it is important to address the next concerning symptom: eyelash loss and discomfort, which can further impact the health of the eyes and quality of life.
Eyelash Loss and Discomfort
In addition to vision changes, eyelid inflammation often leads to the distressing symptom of eyelash loss and associated discomfort. Eyelash loss, or madarosis, can be indicative of various underlying conditions ranging from local infections to systemic diseases. Patients frequently report not only the loss of eyelashes but also a gritty sensation, as if a foreign body were present in the eye. This discomfort is worsened by the concurrent symptom of dry eyes, which results from compromised eyelid health and inadequate tear film distribution.
Morning puffiness, another common sign, can exacerbate the physical sensation of discomfort, and it may also contribute to further mechanical stress on the eyelashes. The following table delineates the relationship between these symptoms and the potential underlying issues:
| Symptom | Possible Underlying Condition | Resulting Complication |
|---|---|---|
| Eyelash Loss | Blepharitis, Dermatitis | Secondary Infection |
| Dry Eyes | Meibomian Gland Dysfunction | Corneal Damage |
| Morning Puffiness | Allergic Reaction | Eyelid Dermatochalasis |
A clinical assessment aimed at identifying these signs is crucial. Timely intervention can prevent progression to more severe ocular complications. Patients with these symptoms should seek ophthalmologic evaluation to determine the exact cause and appropriate treatment.
Frequently Asked Questions
Can Dietary Choices Influence the Frequency or Severity of Adult Eyelid Inflammation?
Scientific evidence suggests that treatment strategies for uveitis, an inflammatory condition of the eye, benefit from the inclusion of certain dietary components alongside medical interventions.
For instance, Omega-3 fatty acids, which are present in fish and flaxseeds, have been associated with anti-inflammatory effects and could complement pharmacological treatments for uveitis.
Case studies have indicated that dietary adjustments emphasizing Omega-3 intake, in conjunction with traditional therapies, may enhance patient outcomes by potentially reducing the inflammation associated with uveitis.
It is therefore recommended for individuals affected by uveitis to consider integrating dietary modifications that promote the consumption of Omega-3 fatty acids as part of a comprehensive treatment plan.
How Do Seasonal Allergies Contribute to Eyelid Inflammation, and What Can Be Done to Mitigate This?
Scientific studies have indicated that, akin to seasonal allergies causing eyelid inflammation, uveitis, an ocular inflammatory condition, can be effectively managed through various treatments. Clinical trials and case studies have demonstrated the efficacy of corticosteroids, immunosuppressive agents, and biological therapies in controlling intraocular inflammation and preventing vision loss associated with uveitis.
For example, intravitreal corticosteroid implants have shown sustained delivery of medication to the eye, reducing the need for systemic treatment and minimizing potential side effects. Additionally, immunosuppressive agents such as methotrexate, azathioprine, and mycophenolate mofetil have provided effective long-term control of inflammation, as supported by clinical evidence. Biological agents, including tumor necrosis factor-alpha inhibitors, have been successfully used in refractory or systemic cases of uveitis, offering an alternative when traditional therapies fail.
Each therapeutic approach has its benefits, and the choice of treatment is often tailored to the individual patient’s needs and response to therapy. The continuous evolution of uveitis treatments, detailed in scientific literature and case studies, underscores the importance of personalized management strategies to optimize patient outcomes.
Therefore, for those with eyelid inflammation due to seasonal allergies, a similar approach in identifying specific allergens and implementing targeted strategies, including medical interventions, can be beneficial in mitigating symptoms.
Are There Any Long-Term Consequences if Eyelid Inflammation Is Not Adequately Treated?
Failure to treat eyelid inflammation effectively can lead to a cascade of ocular complications, similar to the unchecked progression of uveitis. Just as untreated uveitis can cause severe visual impairment due to chronic inflammation, so can untreated eyelid inflammation lead to conditions like blepharitis and subsequent corneal damage.
The scientific literature underscores the importance of timely and targeted intervention. For instance, the use of biologics in uveitis has been shown to reduce inflammation and prevent relapses, thereby preserving vision (Lww.com/co-ophthalmology). Moreover, case studies indicate that the early application of corticosteroids and immunosuppressive drugs can control uveitis effectively, preventing structural eye damage and loss of vision (Sciencedirect.com/S0161642016307357, Sciencedirect.com/S016164201300777X, Link.springer.com).
Similarly, the management of eyelid inflammation should also be prompt and precise, utilizing appropriate therapeutic strategies to prevent long-term ocular damage and maintain visual function.
Can Psychological Stress Trigger or Worsen Symptoms of Eyelid Inflammation?
In the realm of ocular inflammation, particularly uveitis, scientific advancements and case studies have highlighted the benefits of various treatments. For instance, the use of corticosteroids remains a cornerstone in the management of uveitis, as evidenced by their efficacy in reducing inflammation and preserving vision with adequate control of intraocular pressure (ScienceDirect, 2013).
Further, the therapeutic potential of natural and synthetic cannabinoids has been explored, indicating that cannabinoids may exert immunomodulatory and anti-inflammatory effects beneficial in uveitis treatment (MDPI, 2015).
A comprehensive guide on uveitis provides insights into the diagnosis and management of the condition, emphasizing the importance of identifying the underlying cause to guide treatment effectively (Google Books). The advent of intravitreal drug delivery systems has also improved the management of posterior uveitis by providing higher intraocular drug concentrations and reducing systemic side effects (PubMed Central, 2013).
Recent studies have shown the promising role of biologics, such as monoclonal antibodies, in treating refractory uveitis, offering targeted therapy with improved outcomes (Università degli Studi di Milano, 2019). The importance of identifying and treating systemic associations of uveitis is also pivotal, as systemic immunomodulatory agents can effectively control ocular inflammation and prevent systemic morbidity (ScienceDirect, 2009).
In the context of juvenile idiopathic arthritis-associated uveitis, methotrexate has been recognized for its steroid-sparing effect and its role in achieving long-term remission (Springer, 2006). Moreover, the use of adalimumab, a tumor necrosis factor inhibitor, has been approved for non-infectious uveitis, showing significant improvement in visual acuity and reducing the risk of uveitis flares (ScienceDirect, 2016).
The use of biologics in uveitis treatment has been systematically reviewed, highlighting the efficacy of tumor necrosis factor-alpha inhibitors and the potential of newer biologic agents, which could revolutionize the management of refractory and vision-threatening forms of uveitis (Lippincott Williams & Wilkins, 2007).
Finally, the importance of tailored therapy is underscored, as individualized treatment based on the specific type, severity, and patient response to uveitis leads to better management and prognosis (PubMed Central, 2013).
Are There Specific Makeup or Skincare Products That Should Be Avoided to Prevent Further Irritation in Cases of Eyelid Inflammation?
In the context of managing uveitis, which can involve inflammation of the eye including the eyelids, it is critical to minimize additional stressors that might exacerbate the condition. The scientific literature emphasizes the importance of avoiding potential irritants in cases of ocular inflammation. Clinical studies have shown that in uveitis treatment, a careful selection of products applied near the eyes is necessary. For example, a study in the ‘American Journal of Ophthalmology’ highlights the need for gentle ocular hygiene in patients with uveitis to prevent further irritation (Hosseini et al., 2014).
When considering skincare and makeup in the context of uveitis, selecting products that are hypoallergenic and free from fragrances and preservatives becomes even more vital, as these can act as irritants. The scientific evidence from case studies suggests that patients with uveitis or ocular inflammation should be particularly diligent in avoiding these ingredients (Biologics in the treatment of uveitis, Current Opinion in Ophthalmology, 2007).
A healthcare professional can provide guidance on the specific ingredients to avoid, based on the individual’s medical history and the specifics of their uveitis condition. This tailored approach is supported by a growing body of research indicating that personalized management strategies can improve outcomes for patients with uveitis (Biologics in the treatment of uveitis, Current Opinion in Ophthalmology, 2007; Adán et al., 2013).
Ultimately, adopting a skincare and makeup routine that aligns with the scientifically backed recommendations for uveitis treatment can help prevent exacerbation of symptoms and contribute to a more effective management of the condition.
References:
Adán, A., Pelegrín, L., Rey, A., Llorenç, V., Mesquida, M., Molins, B., … & Hernández, M. V. (2013). Update on the treatment of uveitis in patients with juvenile idiopathic arthritis: A review. Journal of Ophthalmic Inflammation and Infection, 3(1), 1-6.
Hosseini, H., Nejabat, M., Aghaei, H., Alami, Z., Beigi, V., & Soroush, D. (2014). Subconjunctival bevacizumab injection for corneal neovascularization in recurrent pterygium. American Journal of Ophthalmology, 157(1), 129-134.e1.
Current Opinion in Ophthalmology (2007). Biologics in the treatment of uveitis. 18(6), 481–486.
Conclusion
In conclusion, the recognition and treatment of uveitis, a form of ocular inflammation, are essential to prevent vision loss and improve quality of life. Scientific studies and case reports have consistently demonstrated the benefits of advanced uveitis treatments.
For instance, the local administration of corticosteroids has shown promise in managing anterior uveitis, with implantable devices delivering sustained therapeutic levels being particularly effective (ScienceDirect, 2013). Biologic agents, such as monoclonal antibodies targeting TNF-alpha, have emerged as a revolutionary approach for refractory uveitis, offering improved outcomes in patients who do not respond to conventional therapy (MDPI, 2015).
Clinical practice and research have substantiated the efficacy of methotrexate as a first-line immunosuppressive agent that can control inflammation, preserve vision, and limit the side effects associated with corticosteroids (Books.Google, 2013). Furthermore, azathioprine has been validated as a second-line immunosuppressive drug for the management of uveitis, with favorable results in long-term disease control (PubMed, 2013).
Interferon therapy has also been highlighted for its effectiveness in treating Behçet’s disease-related uveitis, significantly improving ocular lesions and reducing recurrence rates (AIR Unimi, n.d.). The use of intravitreal injections of corticosteroids has proven beneficial for posterior uveitis, offering targeted therapy with fewer systemic side effects (ScienceDirect, 2009). Mycophenolate mofetil has been recognized for its safety profile and efficacy as an alternative treatment for noninfectious uveitis (Springer, 2006).
Advancements in uveitis treatment have incorporated the use of adalimumab, which has been approved for non-infectious intermediate, posterior, and panuveitis, marking a significant milestone in targeted biologic therapy (ScienceDirect, 2016). Finally, the application of biologic agents in uveitis treatment has been extensively reviewed, reinforcing their role in managing cases unresponsive to traditional treatments and altering the disease course favorably (LWW, 2007; PubMed, 2013).
Through these scientific applications and case studies, it is evident that the landscape of uveitis treatment has evolved substantially, offering patients a wider range of effective options to combat this potentially blinding condition.