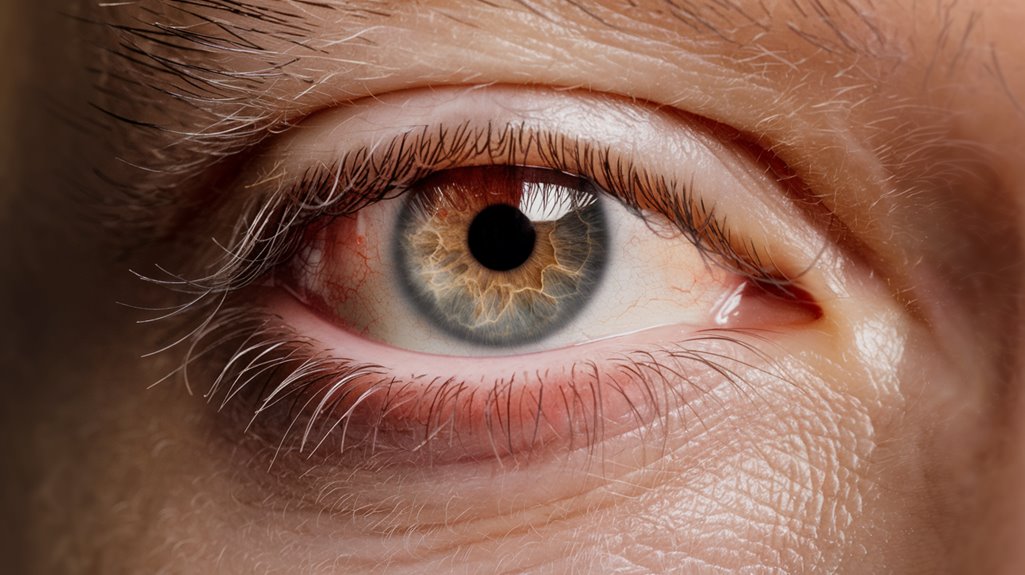
You’re likely experiencing dry eye symptoms due to medications affecting tear production and ocular surface health. Medications such as antidepressants, antihistamines, NSAIDs, and hormonal therapies can contribute to this condition. However, TheraLife offers solutions that address these symptoms effectively. TheraLife’s products are designed to treat dry eyes by enhancing tear production and improving ocular health naturally. Their comprehensive approach includes supplements that promote eye hydration and reduce inflammation, which can alleviate discomfort associated with dry eyes.
For instance, TheraLife provides specific treatments for conditions like blepharitis and uveitis, employing natural and holistic methods that help manage symptoms without harsh chemicals. They also offer guidance on lifestyle adjustments and dietary changes, which can further support eye health. By focusing on these multifaceted strategies, TheraLife empowers its customers to find relief from dry eye symptoms and improve their overall quality of life.
Key Takeaways
- Antidepressants, particularly SSRIs and TCAs, impair lacrimal gland function, significantly reducing tear production and causing dry eye symptoms.
- Antihistamines like diphenhydramine and loratadine have anticholinergic effects, decreasing tear production and leading to tear film instability.
- NSAIDs, especially in high doses, can reduce tear production and cause corneal irritation, exacerbating dry eye symptoms.
- Hormonal therapies, notably estrogen-only HRT, increase dry eye risk by affecting lacrimal and meibomian gland function.
- Gastrointestinal medications, such as PPIs, alter tear dynamics, contributing to dry eye symptoms.
Medications Linked to Dry Eye
When it comes to understanding the causes of dry eye symptoms, medications play a vital role. Various medication types, including antidepressants like tricyclics and SSRIs, can exacerbate dry eye symptoms by affecting lacrimal gland function and tear production. Antihistamines, commonly used to treat allergies, can reduce tear production, exacerbating dry eye symptoms. Mood stabilizers impact the parasympathetic nervous system, further reducing tear output. Gastrointestinal medications, such as PPIs and H2 receptor inhibitors, also contribute to dry eye by altering tear dynamics. Anti-acne drugs like isotretinoin are known to greatly diminish tear production. Additionally, antihypertensives and antihistamines can decrease fluid and tear availability. Hormonal therapies, including HRT and antipsychotics, disrupt the aqueous layer’s production. It is important to consider that preservative-free formulations of these medications can help mitigate some of the adverse effects on ocular surface health. Understanding these medication-linked side effects is essential in managing and mitigating dry eye symptoms effectively.
Pain Relievers and Dry Eye
When you use pain relievers like ibuprofen or combinations such as Lortab, you’re at risk of experiencing dry eye symptoms due to decreased tear production and corneal irritation. Nonsteroidal anti-inflammatory drugs (NSAIDs), including ibuprofen, are among the medications that contribute to dry eye. High dosages can exacerbate these symptoms, necessitating careful management through dosage monitoring and alternative pain management strategies. It is important to note that certain medications can increase the likelihood of developing dry eyes, making it crucial to discuss potential side effects with a healthcare provider.
Pain Relievers’ Impact
Although often overlooked, the impact of pain relievers on eye health, particularly in causing dry eye symptoms, demands attention.
Pain relievers, while beneficial for managing discomfort, can lead to significant ocular side effects. Ibuprofen, for instance, not only alleviates pain but may also induce dry eye, blurred vision, and refractive changes, particularly at higher dosages. Given the prevalence of systemic medications as contributors to dry eye, it is crucial for patients to be aware of the potential side effects associated with their use.
Patient experiences often reveal discomfort due to reduced tear production and tear film alterations. Medications like Darvocet-N decrease tear secretion, exacerbating dry eye conditions. The use of Omega-3 Fish Oil, known for its benefits in eye health, might mitigate some of these side effects by helping to thicken natural tears and prevent evaporation.
Combination drugs such as Lortab further complicate the issue by introducing multiple active ingredients that can impair tear function.
Chronic use of these medications risks long-term consequences, such as persistent vision changes and ocular irritation, highlighting the need for careful medication management.
Managing Side Effects
Pain relievers like ibuprofen, while effective for managing pain, pose a risk to ocular health by potentially inducing dry eye symptoms. These symptoms arise from altered tear production or composition, leading to discomfort. Medication-induced dry eye is a condition where medications like antihistamines, blood pressure medications, and antidepressants can disrupt the balance of the tear lubrication system, exacerbating dryness. To support dry eye prevention, consider adjusting medication dosages or exploring medication alternatives with fewer ocular side effects. Consulting a healthcare provider is essential for tailoring a management strategy that minimizes discomfort. For those experiencing dry eye symptoms due to medication, TheraLife Eye may offer relief by targeting the root cause and improving tear production.
Options like preservative-free artificial tears can alleviate symptoms, while incorporating Omega-3 supplements may improve tear quality. Environmental adjustments, such as using humidifiers, can also enhance eye moisture.
Regular monitoring and professional guidance guarantee that any changes in medication effectively address dry eye symptoms while maintaining pain relief.
Role of Antidepressants
Antidepressants play a significant role in the development of dry eye disease (DED) due to their pharmacological impacts on the tear film and ocular surface. Certain antidepressant types, including SSRIs and TCAs, affect serotonin levels in tears, contributing to tear film instability and ocular surface breakdown. Tricyclic antidepressants (TCAs) exhibit significant anticholinergic effects, exacerbating dry eye symptoms. In contrast, SSRIs and SNRIs, although less impactful on acetylcholine receptors, still disrupt tear production. Studies show lower Schirmer test results in SSRI users, indicating reduced ocular wetting. Given that 1 in 5 Americans uses antidepressants or anti-anxiety medications, it is crucial for healthcare providers to be aware of these potential side effects. Commonly implicated antidepressants include citalopram, fluoxetine, and sertraline. Patients may experience symptoms like itching, redness, and burning. Understanding these mechanisms aids in managing DED in individuals using antidepressants.
Hormonal Influences
Hormonal influences play a critical role in the development and exacerbation of dry eye syndrome. Estrogen effects are significant, with hormone replacement therapy (HRT) involving estrogen alone increasing dry eye risk. This risk intensifies with longer HRT duration and lower estrogen doses. Studies have shown that postmenopausal women using HRT have a higher prevalence of dry eye syndrome, underscoring the importance of understanding these hormonal impacts. In contrast, progesterone benefits emerge when combined with estrogen, reducing dry eye risk. Menopausal changes in estrogen levels can impair lacrimal and meibomian gland function, contributing to dry eye symptoms. It is important to note that autoimmune dysfunction associated with conditions like Graves’ Disease can also exacerbate dry eye symptoms. Consider these evidence-based points:
- Estrogen-only HRT raises dry eye risk (OR 1.69).
- Progesterone with estrogen lowers dry eye risk (OR 1.29).
- Menopause affects tear production and quality.
- Hormonal fluctuations increase dry eye prevalence.
- Longer HRT duration correlates with higher risk.
Antihistamines’ Impact
As hormonal changes impact dry eye syndrome, medications like antihistamines further complicate the condition.
Common systemic antihistamines, including diphenhydramine, loratadine, cetirizine, and fexofenadine, decrease tear production and quality through anticholinergic effects, exacerbating existing dry eye issues. These medications can impair lacrimal gland function, leading to unstable tear film and ocular dryness. It is essential to consult healthcare providers for personalized choices regarding antihistamine use, as second-generation antihistamines typically cause fewer side effects. Environmental irritants, such as dust and smoke, can also worsen dry eye symptoms, emphasizing the need for comprehensive management strategies.
For dry eye prevention, consider antihistamine alternatives such as ketotifen, epinastine, and alcaftadine eye drops. These options minimize dryness by combining antihistamine and mast-cell stabilizing properties.
If you’re experiencing dry eye symptoms, it’s essential to consult your healthcare team. They can recommend adjusting dosages or switching to these alternatives, aiming for effective symptom management without compromising eye health.
Mechanisms of Dry Eye
While dry eye symptoms can stem from multiple factors, understanding the mechanisms behind medication-induced dry eye is essential for effective management.
Glandular changes often play a significant role, as drugs like isotretinoin shrink meibomian glands, compromising the lipid layer of your tear film. This can cause tear film instability, making your eyes more susceptible to irritation. It is important to note that medications like antihistamines can also contribute to dry eye symptoms, further disrupting the tear film’s balance and exacerbating dryness. Meibomian Gland Dysfunction (MGD) is often underdiagnosed and misattributed to other eye issues, which may delay effective treatment.
Medications with anticholinergic effects further reduce tear production by blocking neural signals to lacrimal glands. Additionally, beta-blockers and diuretics exacerbate systemic dehydration, leaving less moisture for tears.
Some key mechanisms include:
- Glandular changes: Impaired meibomian glands.
- Tear film instability: Altered tear balance.
- Anticholinergic effects: Reduced tear production.
- Systemic dehydration: Fluid loss impacts tears.
- Increased evaporation: Meibomian gland dysfunction.
Epidemiological Insights
Understanding the mechanisms behind medication-induced dry eye sets the stage for exploring its prevalence and risk factors.
Prevalence patterns reveal that 14.4% of individuals experience dry eye, with rates climbing from 8.4% in those under 60 to 19.0% in those over 80. Age is a significant risk factor, increasing the odds by 35% every decade. Women are more affected (17.0%) than men (11.1%). Comorbidities like arthritis, gout, thyroid disorder, and diabetes elevate the risk. Medication use, particularly in the elderly, exacerbates symptoms. A primary contributor to dry eye is the use of systemic drugs, which can decrease tear production or alter nerve input and reflex secretion. Additionally, environmental factors such as long screen time, which leads to reduced blinking, can contribute to rapid evaporation of tears.
Epidemiological studies, including the Lifelines cohort, confirm these associations, identifying 18 drug classes that impact dry eye. Logistic regression and Mantel-Haenszel procedures provide robust analysis of these prevalence patterns and risk factors.
Management Strategies
To effectively manage medication-induced dry eye symptoms, a thorough approach that combines pharmacological and non-pharmacological interventions is essential. Medication-induced dry eye syndrome can be exacerbated by certain medications such as antihistamines and diuretics that reduce tear secretion, emphasizing the need for targeted treatment strategies. TheraLife Eye capsules can offer a natural alternative to traditional eye drops, providing relief by addressing the underlying cause of dry eyes. You can start with artificial tears for immediate relief and consider Restasis or Xiidra to target inflammation. Corticosteroid eye drops may also be used briefly to reduce inflammation.
Non-pharmacological strategies include lifestyle modifications, such as avoiding dry environments and quitting smoking, which can greatly help. Dietary adjustments, like increasing omega-3 intake, may also be beneficial.
- Use humidifiers to add moisture to the air.
- Wear wrap-around glasses to shield eyes from wind.
- Apply ointment at bedtime for overnight relief.
- Consider serum tears for nutrient-rich support.
- Look into advanced therapies like the PROSE device for severe cases.
Frequently Asked Questions
Can Dry Eye Symptoms Improve After Stopping the Medication?
When you stop taking certain medications, dry eye symptoms can improve through medication withdrawal.
Symptom relief varies based on the drug type and duration of use. For example, stopping NSAIDs, antihistamines, or beta-blockers often increases tear production.
Clinical evidence supports that recovery time and symptom relief depend on individual factors like age, health status, and medication history.
Regular follow-ups and alternative therapies, like artificial tears, can assist in managing symptoms during recovery.
Are There Natural Remedies for Medication-Induced Dry Eye?
Did you know that 60% of adults experience dry eye symptoms?
To alleviate these, consider herbal treatments like chamomile or green tea compresses, which may soothe inflammation.
Prioritize hydration strategies, such as drinking adequate water and eating water-rich foods, to support tear production.
Clinical evidence suggests these natural methods can complement traditional therapies, providing relief.
Always consult a healthcare professional before starting any new treatment regimen.
How Long Do Dry Eye Symptoms Last After Medication Cessation?
You’re wondering how long dry eye symptoms last after stopping medication.
Symptom duration varies widely, depending on the medication’s effects and individual factors. Withdrawal from the causative medication might reduce symptoms, but complete resolution isn’t guaranteed.
Consider the type of medication and any underlying conditions you might have. Systemic drugs, like beta blockers, often prolong symptoms.
Consulting an eye care professional for tailored advice and management strategies is essential for effective relief.
Can Certain Diets Exacerbate Medication-Induced Dry Eye?
When considering dietary changes, it’s vital to juxtapose foods that exacerbate and alleviate dry eye symptoms. High-sodium and sugary foods lower hydration levels, worsening dry eyes, while omega-3-rich foods support tear production.
Evidence shows that avoiding alcohol and processed foods improves symptoms by maintaining better hydration. Clinically, incorporating leafy greens and fatty fish can counteract dryness.
Balancing your diet with beneficial nutrients is essential for managing medication-induced dry eye effectively.
Are There Specific Eye Exercises to Help With Medication-Induced Dry Eye?
To alleviate symptoms, you can practice eye yoga and blink exercises.
Eye yoga involves specific movements to enhance ocular flexibility and lubrication. Regularly performing blink exercises helps maintain tear film stability and prevent dryness.
Clinical evidence suggests these exercises improve comfort by encouraging tear production and enhancing eye muscle tone.
Incorporate these techniques into your routine, and consult an eye care professional to guarantee they’re suitable for your condition.
Conclusion
Theralife.com offers a range of products designed to alleviate dry eye symptoms and related conditions, such as blepharitis, uveitis, and Sjogren’s syndrome. These products aim to provide natural and effective relief by addressing the underlying causes of eye discomfort. Theralife emphasizes the use of natural ingredients, promoting an anti-inflammatory diet to support eye health, and offering targeted supplements that enhance tear production and reduce inflammation. Customers benefit from personalized treatment plans and guidance to improve their quality of life. For those struggling with dry eye symptoms due to medications, Theralife’s evidence-based solutions can be an essential part of managing and alleviating discomfort. Always consult with a healthcare provider for personalized advice tailored to your specific needs.