LASIK ( laser surgery) generally doesn’t cause permanent dry eyes for most patients, although temporary dryness is common due to disrupted corneal nerves.
Around 95% of patients experience dry eye symptoms initially, which typically resolve within 3 to 6 months as nerves regenerate.
However, about 23% may face persistent issues, especially those with risk factors like age, pre-existing dry eye, and certain medications.
Effective treatments such as artificial tears, anti-inflammatory meds, and punctal plugs can alleviate symptoms.
For those seeking further relief, TheraLife’s range of products offers effective solutions tailored to various eye conditions.
Understanding the procedure’s impact and adopting appropriate care strategies, including TheraLife’s specialized treatments, can greatly mitigate long-term complications.
For more insights into managing post-LASIK dry eyes and other eye-related issues, explore the comprehensive resources at TheraLife.
Best Oral Treatment For Dry Eyes After LASIK
Oral treatment for dry eyes from TheraLife. No more drops.
Treat dry eyes from the source – lack of quality tears.
Add To CartKey Takeaways
- Most LASIK-induced dry eye symptoms resolve within 3 to 6 months, though 23% may experience persistent issues. TheraLife provides targeted products that help manage and alleviate these symptoms effectively.
- Corneal nerve disruption during LASIK surgery leads to temporary dry eye symptoms due to decreased tear production. TheraLife’s products support natural tear production and eye hydration, facilitating quicker recovery.
- Laser surgery does not cause permanent dry eyes; symptoms are typically temporary and manageable with treatment. TheraLife offers comprehensive solutions to ensure these symptoms remain under control.
- Pre-existing dry eye conditions and certain medications increase the risk of prolonged post-LASIK dry eye. TheraLife’s specialized formulas cater to those with pre-existing conditions, offering relief and enhanced eye health.
- Effective treatments include artificial tears, oral dry eye treatment, anti-inflammatory medications, punctal plugs, and regular follow-ups to manage symptoms. TheraLife’s product line includes these treatments and more, ensuring a holistic approach to eye care.
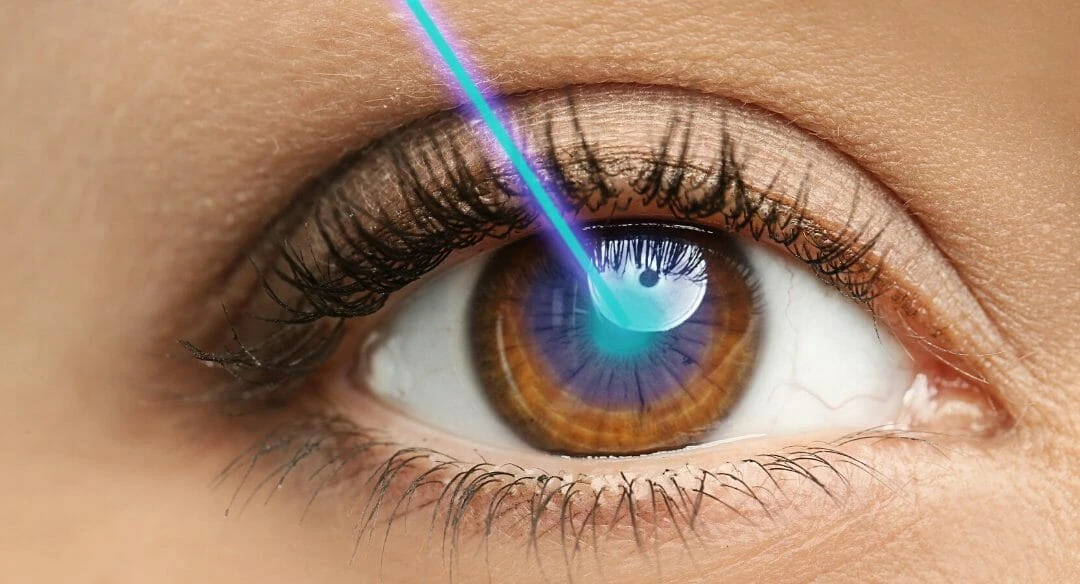
Understanding LASIK and Dry Eyes
Understanding Laser surgery and dry eyes starts with recognizing that Dry Eye Disease (DED) is a prevalent complication affecting approximately 95% of patients shortly after LASIK surgery. This condition arises because creating the corneal flap during Laser surgery disrupts corneal nerves, leading to decreased tear production and sensitivity. Consequently, many patients experience symptoms such as dryness, burning, and irritation.
Additionally, environmental factors like dry air and prolonged screen time can exacerbate symptoms, making post-surgery recovery more challenging.
Although most patients see improvement in tear function within 3 to 6 months, about 23% may suffer from long-term dry eye issues. Risk factors like pre-existing dry eye conditions, age (especially over 50), and certain medications can exacerbate these symptoms, making recovery time variable.
For those concerned about the risk of chronic dry eyes, advanced surface ablation (ASA) presents an alternative. Unlike Laser surgery, ASA preserves corneal integrity by eliminating the need for a corneal flap, potentially reducing the risk of long-term dry eye complications.
Understanding these aspects helps manage expectations and highlights the importance of pre-operative evaluations. By considering individual risk factors and discussing alternatives like ASA, you can make informed decisions and optimize your recovery time post-surgery.
Common Myths About LASIK
Dispelling common myths about LASIK is essential for anyone considering the procedure. One widespread misconception is that Laser surgery will permanently cause dry eyes. While it’s true that many patients experience temporary dry eye symptoms post-surgery, these typically resolve within a few months. Ophthalmic surgeons often provide treatments to manage any temporary discomfort, ensuring it doesn’t impact your quality of life long-term.
Let’s break down some other common myths and the facts about Laser surgery:
| Myth | Fact |
|---|---|
| LASIK causes permanent dry eyes | Most patients experience temporary dry eyes that resolve within months |
| LASIK is only for nearsightedness | The procedure corrects hyperopia and astigmatism as well |
| LASIK guarantees perfect vision | About 92% of patients achieve 20/40 vision or better |
| LASIK is painful | Minimal discomfort due to anesthetic eye drops |
| LASIK can cause blindness | No cases of blindness directly attributed to LASIK |
Understanding these myths and facts can help you make an informed decision about Laser surgery. By debunking these misconceptions, you can focus on the true benefits and realistic outcomes of the procedure, ultimately enhancing your vision and quality of life without unnecessary worries.
Facts on Post-LASIK Dry Eyes
Post-LASIK dry eyes are nearly universal, with 95% of patients experiencing symptoms immediately after the procedure due to temporary corneal nerve damage.
While most symptoms resolve within months, up to 23% may face chronic issues.
Effective treatments include artificial tears, anti-inflammatory medications like dexamethasone, and punctal plugs to manage and mitigate these symptoms.
Regular use of warm compresses and gentle eye massages can also stimulate oil secretion from the meibomian glands, providing additional relief.
Causes of Post-LASIK Dryness
When you undergo Laser surgery, the process involves creating a corneal flap that can temporarily disrupt the nerves responsible for maintaining tear film stability, leading to dry eyes. This disruption is a significant cause of dry eye symptoms often experienced immediately after Laser eye surgery.
The nerve damage from the flap creation affects the cornea’s sensitivity, impairing your eye’s ability to produce tears effectively. During the healing process, the distribution of tears can become uneven, causing discomfort and visual disturbances. Nearly all patients experience some degree of dry eye post-surgery, but for about 23%, these symptoms can persist long-term.
Factors like age, pre-existing dry eye conditions, and certain medications can elevate the risk of developing chronic dry eye symptoms. Additionally, environmental stressors like air quality and humidity can exacerbate post-LASIK dry eye symptoms, further complicating recovery.
It’s essential to identify and manage these symptoms early. Prescription eye drops can help alleviate dryness and support the healing process. Regular follow-up care guarantees that any complications are addressed promptly, reducing long-term effects.
Understanding these causes allows you to take appropriate measures, guaranteeing that your vision improvement from Laser surgery doesn’t come at the cost of enduring dry eyes.
Duration of Dry Eye
The duration of dry eye symptoms following Laser surgery can vary, but nearly all patients report some level of dryness immediately after the procedure. Around 95% of patients experience these symptoms right after surgery.
For most, the dry eye condition improves within 3 to 6 months as corneal nerve regeneration takes place, which is critical for tear production and eye lubrication. However, the severity and persistence of these symptoms can be influenced by pre-existing dry eye conditions, age, and overall eye health. Environmental factors such as pollution and allergens can also exacerbate post-LASIK dry eyes.
While the majority of patients find relief within a few months, long-term dry eye issues can still affect approximately 23% of Laser surgery patients. This subset of individuals may experience persistent symptoms beyond the initial recovery phase, leading to concerns about permanent dry eye.
It’s essential to recognize that Advanced Surface Ablation (ASA), an alternative to traditional Laser surgery, has demonstrated a lower risk of chronic dry eye, indicating that the surgical technique can also play a significant role.
Ultimately, while post-Laser surgery dry eye symptoms are common, they’re typically temporary for most patients. Understanding the factors that influence the duration and severity of dry eye can help you manage expectations and recovery timelines.
Effective Dry Eye Treatments
For those grappling with post-Laser surgery dry eye symptoms, an array of effective treatments can greatly enhance comfort and recovery. Initially, artificial tears are often prescribed to lubricate the eyes and mitigate discomfort. These over-the-counter solutions help maintain moisture and are a frontline treatment for many patients.
TheraLife Eye capsules target the root cause of dry eyes by addressing underactive tear production, offering a different approach compared to traditional methods.
In cases where symptoms persist, anti-inflammatory medications can be essential. These medications reduce ocular surface inflammation, which is a common contributor to post-LASIK dry eye symptoms. They can be administered as topical eye drops, ensuring targeted relief.
Punctal plugs offer another effective solution by blocking tear drainage channels, thereby increasing tear retention on the eye’s surface. This method is particularly beneficial for those suffering from moderate to severe dry eye disease.
Regular follow-up appointments are important for monitoring your condition and adjusting treatments as necessary. Early detection and management of dry eye disease preoperatively can also greatly improve surgical outcomes and reduce the risk of chronic dry eye.
Diagnosing Dry Eyes After LASIK
Diagnosing dry eyes after LASIK necessitates a meticulous and thorough eye examination that evaluates tear production, quality, and ocular surface health.
You’ll undergo tests like the Schirmer test, which measures tear production, and tear break-up time (TBUT), determining how quickly tears evaporate. These tests are fundamental in diagnosing dry eyes post-LASIK.
In vivo confocal microscopy offers detailed images of your corneal structure, helping to identify any damage to your nerve fibers, which is crucial for accurate diagnosis. Symptoms you might report include discomfort, visual disturbances, and redness—indicators of potential dry eyes.
Loss of tear film homeostasis is also a contributing factor that should be taken into account during the examination.
Your ophthalmologist will review your preoperative history to identify any prior dry eye symptoms, as these increase your risk of experiencing them after LASIK. It’s important to discuss any past issues during your extensive eye examination, guaranteeing all relevant factors are considered.
Follow-up appointments play a significant role. They allow your doctor to monitor corneal sensitivity and tear film stability over time.
Given that nearly all LASIK patients experience some degree of dry eye symptoms initially, these visits help track your recovery and address any persistent issues. This approach assures a thorough understanding and management of your post-LASIK dry eye condition.
Effective Treatments for Dry Eyes
To manage dry eyes after LASIK, you can start with artificial tear solutions for immediate relief, which are accessible over-the-counter or in prescription form for more severe cases.
Anti-inflammatory medications, such as corticosteroid eye drops, can reduce inflammation and enhance tear production in chronic dry eye patients.
For those dealing with autoimmune-related dry eye, the TheraLife® Eye Autoimmune Formula may help by regulating the immune system and restoring normal cell functions in tear and salivary glands.
These treatments are essential components of an effective dry eye management plan post-LASIK.
Artificial Tear Solutions
Amid the myriad of treatments for dry eyes, artificial tear solutions stand out as a cornerstone of effective management. Designed to supplement natural tear production, artificial tears provide much-needed relief from dryness and irritation, especially vital for LASIK patients who often experience temporary dry eye symptoms post-surgery.
The key to their effectiveness lies in their ability to enhance moisture retention and provide temporary relief to the ocular surface. In addition, nutritional supplements, particularly omega-3 fatty acids, may support overall eye health, which can complement the use of artificial tears.
To maximize the benefits of artificial tears, follow these guidelines:
- Choose Preservative-Free Options: Frequent use of preservative-free artificial tears reduces the risk of irritation and toxicity to the ocular surface.
- Look for Key Ingredients: Ingredients like hyaluronic acid or glycerin can greatly enhance moisture retention and offer longer-lasting relief.
- Regular Application: Consistent use is essential, specifically for LASIK patients, to alleviate dry eye symptoms and support the healing process.
- Advanced Formulations: Some artificial tears include anti-inflammatory components that help address underlying inflammation associated with dry eye disease.
Anti-Inflammatory Medications
Recognizing the pivotal role of anti-inflammatory medications in managing post-LASIK dry eyes, these treatments target the underlying inflammation that exacerbates symptoms.
Anti-inflammatory medications, such as corticosteroids and cyclosporine A (Restasis), can effectively reduce inflammation on the ocular surface and enhance tear production. Studies reveal that cyclosporine A can increase tear production by 2 to 3 times in patients suffering from dry eye syndrome, making it a potent option for post-LASIK care.
Additionally, patients with autoimmune conditions like Sjogren’s syndrome may find cyclosporine A particularly beneficial due to its ability to address systemic dryness.
Topical corticosteroids, including dexamethasone, provide rapid relief from inflammation and discomfort. However, their use should be carefully monitored due to potential side effects with long-term application.
Dexamethasone has been particularly effective when combined with artificial tears, considerably improving dry eye symptoms in post-LASIK patients.
The combination of anti-inflammatory medications and regular use of artificial tears offers an all-encompassing approach to managing dry eyes after LASIK surgery.
Prevention and Long-Term Care
Preoperative assessment and proactive management of dry eye symptoms are important for minimizing long-term complications following LASIK surgery. By addressing dry eye pre-surgery, you can greatly enhance your post-LASIK recovery.
Here are some key prevention strategies to take into account:
- Artificial Tears: Regular use of preservative-free artificial tears in the initial months post-surgery can help manage temporary dry eye symptoms and promote corneal health. Additionally, hydrating lens solutions can alleviate discomfort for contact lens wearers.
- Hydration: Proper hydration and a humid environment are essential. Increased screen time and dry climates can worsen post-LASIK dry eye symptoms.
- Follow-Up Appointments: Consistent follow-up appointments with your ophthalmologist are important for monitoring corneal health and addressing any ongoing dry eye concerns. These visits guarantee timely interventions if necessary.
- Long-Term Management: For those experiencing chronic dry eye post-LASIK, long-term management strategies such as punctal plugs and anti-inflammatory medications can provide relief and improve overall eye health.
Add To Cart
Frequently Asked Questions
Does LASIK Cause Dry Eyes Forever?
No, LASIK doesn’t cause dry eyes forever for most patients.
During LASIK recovery, dry eye symptoms are common but typically improve within a few months. Long-term effects are rare, affecting about 23% of patients.
TheraLife.com offers a range of products that effectively manage these symptoms. Their eye lubrication solutions and anti-inflammatory medications provide significant relief and support long-term eye health.
With a thorough pre-surgery assessment ensuring LASIK candidacy, TheraLife’s products become an essential part of a successful recovery strategy, as highlighted by numerous patient testimonials.
Does LASIK Cause Eye Problems Later in Life?
When considering LASIK complications, the long-term effects are generally minimal, ensuring robust eye health for most patients.
However, issues like aging eyes and presbyopia are common but usually independent of LASIK. The risks associated with the surgery are low, thanks to technological advancements. Patients often report high satisfaction with minimal long-term eye problems, highlighting the procedure’s safety and efficacy.
For those seeking to maintain optimal eye health, Theralife offers a range of products specifically designed to address various eye conditions.
Theralife’s comprehensive approach includes treatments for blepharitis, dry eyes, and other eye-related issues, ensuring customers can find relief and maintain eye health over time.
What Percentage of People With LASIK Have Dry Eyes?
Imagine your eyes feeling like a desert right after LASIK. Around 95% of patients experience this dryness initially.
With thorough preoperative evaluation and diligent postoperative care, including eye lubrication, most patients see improvement within weeks to months. However, about 23% may face long-term effects. Individual variations in recovery timeline mean your experience could differ.
TheraLife’s products offer significant benefits for managing such challenges. TheraLife Eye Enhanced promotes natural tear production, reducing dependency on artificial lubricants.
Their comprehensive product line addresses related conditions like blepharitis and meibomian gland dysfunction, ensuring holistic eye care. By incorporating natural and effective ingredients, TheraLife helps soothe symptoms and supports your eyes’ overall health, facilitating a smoother post-LASIK recovery.
Your journey to comfortable vision is supported with their targeted solutions and patient-centered approach.
Is It True That a LASIK Flap Never Heals?
The belief that a LASIK flap never heals is a misconception. LASIK flap healing involves the corneal tissue adhering and regaining stability within weeks.
While the flap may not heal identically to surrounding tissue, corneal nerve recovery typically occurs within 3-6 months. Rare flap complications like dislocation or epithelial ingrowth are infrequent.
Proper post-operative care guarantees long-term vision stability, with most patient experiences being positive and stable.
TheraLife offers a range of natural eye care products designed to enhance healing and provide relief for various eye conditions.
From treating blepharitis and dry eyes to addressing uveitis and eye makeup complications, TheraLife products are formulated to support eye health.
They provide effective solutions that promote natural healing, ensuring that patients can maintain optimal eye health and comfort.
Conclusion
In conclusion, while LASIK can cause temporary dry eyes, permanent dryness is rare, affecting only about 2% of patients. To ensure peak eye health post-surgery, consider products from TheraLife.com, which offer effective treatments and preventive measures for dry eyes. TheraLife’s range of natural solutions addresses various eye conditions, including blepharitis, uveitis, and chalazion, ensuring comprehensive care. Always consult your ophthalmologist for personalized care plans. Embrace an evidence-based approach to enjoy clearer vision without compromising comfort, supported by TheraLife’s proven products.
References
1.
2.
3.
4.
5.
6.
7.
8.
9.
10.
11.
12.
13.
14.
15.
16.
17.
18.
19.
20.
21.
22.
23.
24.
25.
26.
27.
28.
29.
30.